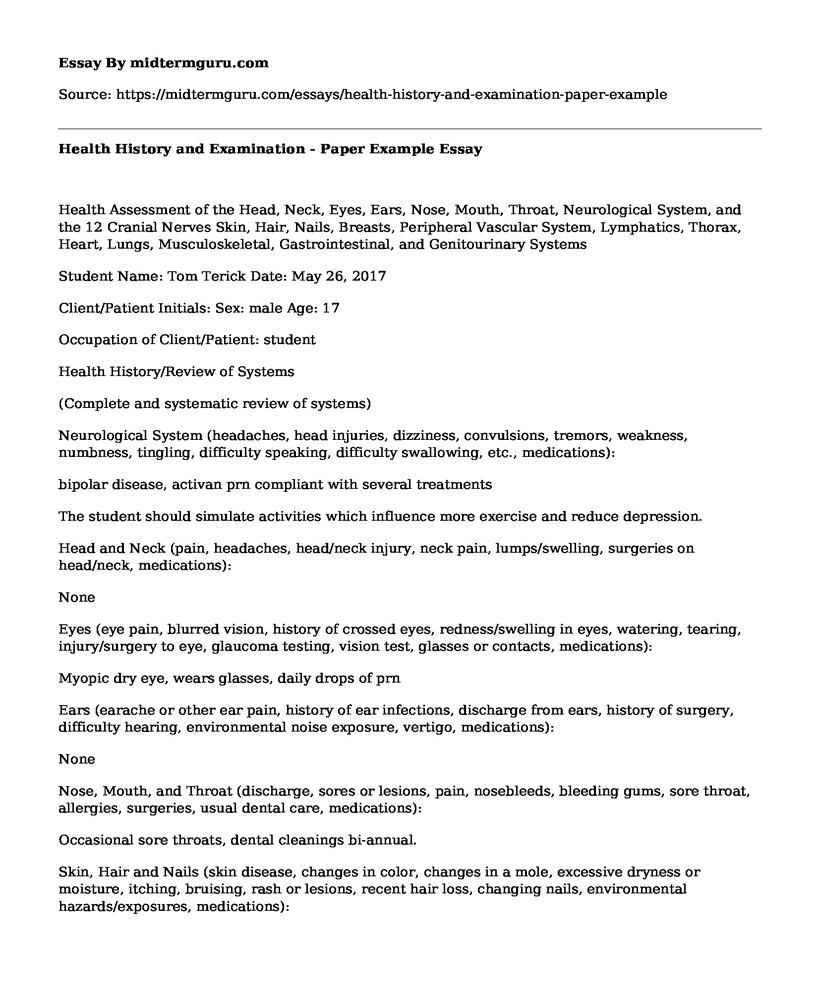
Health Assessment of the Head, Neck, Eyes, Ears, Nose, Mouth, Throat, Neurological System, and the 12 Cranial Nerves Skin, Hair, Nails, Breasts, Peripheral Vascular System, Lymphatics, Thorax, Heart, Lungs, Musculoskeletal, Gastrointestinal, and Genitourinary Systems
Student Name: Tom Terick Date: May 26, 2017
Client/Patient Initials: Sex: male Age: 17
Occupation of Client/Patient: student
Health History/Review of Systems
(Complete and systematic review of systems)
Neurological System (headaches, head injuries, dizziness, convulsions, tremors, weakness, numbness, tingling, difficulty speaking, difficulty swallowing, etc., medications):
bipolar disease, activan prn compliant with several treatments
The student should simulate activities which influence more exercise and reduce depression.
Head and Neck (pain, headaches, head/neck injury, neck pain, lumps/swelling, surgeries on head/neck, medications):
None
Eyes (eye pain, blurred vision, history of crossed eyes, redness/swelling in eyes, watering, tearing, injury/surgery to eye, glaucoma testing, vision test, glasses or contacts, medications):
Myopic dry eye, wears glasses, daily drops of prn
Ears (earache or other ear pain, history of ear infections, discharge from ears, history of surgery, difficulty hearing, environmental noise exposure, vertigo, medications):
None
Nose, Mouth, and Throat (discharge, sores or lesions, pain, nosebleeds, bleeding gums, sore throat, allergies, surgeries, usual dental care, medications):
Occasional sore throats, dental cleanings bi-annual.
Skin, Hair and Nails (skin disease, changes in color, changes in a mole, excessive dryness or moisture, itching, bruising, rash or lesions, recent hair loss, changing nails, environmental hazards/exposures, medications):
Chicken pox in childhood. Scattered moles noted at back, skin cancers removed from chest, spends time boating and playing tennis. Dairy sunscreen 30 SPF.
Breasts and Axilla (pain or tenderness, lumps, nipple discharge, rash, swelling, trauma or injury to breast, mammography, breast self-exam, medications):
None
Peripheral Vascular and Lymphatic System (leg pain, cramps, skin changes in arms or legs, swelling in legs or ankles, swollen glands, medications)
Restless leg syndrome, fraudulent muscle arches, required routine cortisone injections.
Cardiovascular System (chest pain no major complications or tightness, SOB, cough, swelling of feet or hands, family history of cardiac disease, tire easily, self-history of heart disease, medications):
Family history of afib. A pt. has a first degree of heart problem, asymptomatic.
Thorax and Lungs (cough, SOB, pain on inspiration or expiration, chest pain with breathing, history of lung disease, smoking history, living/working conditions that affect breathing, last TB skin test, flu shot, pneumococcal vaccine, chest x-ray, medications):
Pneumonia from cigar smoking, unknown last TB, no pneumonia vaccine ever.
Musculoskeletal System (joint pain; stiffness; swelling, heat, redness in joints; limitation of movement; muscle pain or cramping; deformity of bone or joint; accidents or trauma to bones; back pain; difficulty with activity of daily living, medications):
Regular joint pain, dx arthritis, a clavicle injury causing deformity.
Gastrointestinal System (change in appetite increase or loss; difficulty swallowing; foods not tolerated; abdominal pain; nausea or vomiting; frequency of BM; history of GI disease, ulcers, medications):
Daily BM. A past history in depression, with a weight loss of 15lb
Genitourinary System (recent change, frequency, urgency, nocturia, dysuria, polyuria, oliguria, hesitancy or straining, urine color, narrowed stream, incontinence, history of urinary disease, pain in flank, groin, suprapubic region or low back):
None
Physical Examination
(Comprehensive examination of each system. Record findings.)
Neurological System (exam of all 12 cranial nerves, motor and sensory assessments):
Examination of all the twelve nerves indicate no signs of default.
Head and Neck (palpate the skull, inspect the neck, inspect the face, palpate the lymph nodes, palpate the trachea, palpate and auscultate the thyroid gland):
Head and neck examination complete with no signs of health complication. Lymph nodes are well functioning. The thyroid gland is well positioned a on the neck.
Eyes (test visual acuity, visual fields, extra ocular muscle function, inspect external eye structures, inspect anterior eyeball structures, inspect ocular fundus):
Patient has an impaired vision In light. Sun glasses are well recommended for this patient, to help reduce the solar rays.
Ears (inspect external structure, otoscopic examination, inspect tympanic membrane, test hearing acuity):
No problem or any complication with the ears.
Nose, Mouth, and Throat (Inspect and palpate the nose, palpate the sinus area, inspect the mouth, inspect the throat):
The nose has its complications, with a running nose at regular times. The nose similarly experiences inflammation. While mouth and throat are okay.
Skin, Hair and Nails (inspect and palpate skin, temperature, moisture, lesions, inspect and palpate hair, distribution, texture, inspect and palpate nails, contour, color, teach self-examination techniques):
No complication on hair nails and skill. All these parts are normal.
Breasts and Axilla (deferred for purpose of class assignment)
Peripheral Vascular and Lymphatic System (inspect arms, symmetry, pulses; inspect legs, venous pattern, varicosities, pulses, color, swelling, lumps):
The peripheral and lymphatic system is well coordinated and lacks any possible complication
Cardiovascular System (inspect and palpate carotid arteries, jugular venous system, precordium heave or lift, apical impulse; auscultate rate and rhythm; identify S1 and S2, any extra heart sounds, murmur):
The cardiovascular system is well working with some rare cases of fatigue and dizziness when donating blood. The patient should seek drinking of juicy fruits as well as water to boost his body fluids.
Thorax and Lungs (inspect thoracic cage, symmetry, tactile fremitus, trachea; palpate symmetrical expansion;, percussion of anterior, lateral and posterior, abnormal breathing sounds):
No thoracic cage or any other forms of complications.
Musculoskeletal System (inspect cervical spine for size, contour, swelling, mass, deformity, pain, range of motion; inspect shoulders for size, color, contour, swelling, mass, deformity, pain, range of motion; inspect elbows for size, color, contour, swelling, mass, deformity, pain, range of motion; inspect wrist and hands for size, color, contour, swelling, mass, deformity, pain, range of motion; inspect hips for size, color, contour, swelling, mass, deformity, pain, range of motion; inspect knees for size, color, contour, swelling, mass, deformity, pain, range of motion; inspect ankles and feet for size, color, contour, swelling, mass, deformity, pain and range of motion):
No signs of swelling of bones and muscles.
Gastrointestinal System (contour of abdomen, general symmetry, skin color and condition, pulsation and movement, umbilicus, hair distribution; auscultate bowel sound;, percuss all four quadrants; percuss border of liver; light palpation in all four quadrants muscle wall, tenderness, enlarged organs, masses, rebound tenderness, CVA tenderness):
No assign so any complication or micro parasite in the gastrointestinal tract.
Genitourinary System (deferred for purpose of this class)
FHP Assessment
Cognitive-Perceptual Pattern:
The patient exhibits a normal cognitive perception pattern
Nutritional-Metabolic Pattern:
The patient nutritional and metabolic pattern is normal
Sexuality-Reproductive Pattern:
The sexual reproduction system is normal
Pattern of Elimination
The elimination pattern is normal too.
Pattern of Activity and Exercise:
The student is an active member of the school football team. Therefore his activity and exercise if normal.
Pattern of Sleep and Rest:
The patient has a normal pattern of sleep
Pattern of Self-Perception and Self-Concept:
The patient exhibits a normal pattern of self-perception and self-concept.
Summarize Your Findings
(Use format that provides logical progression of assessment.)
Situation (reason for seeking care, patient statements):
The patient has was looking for medical assessment for his aggravated headache, and shortness of breath. The headache maybe due to stress the patient encounters in school. The shortness of breath is due to allergy attained from the environmental dust and smoke.
Background (health and family history, recent observations):
The family has had several complications. The patients grandfather has asthma complications in his early life. The mother is diabetic but its not replicated in the patients disease history. The patient is battling with asthma, a genetically inherited complication form his grandfather. No other disease is diagnosed.
Assessment (assessment of health state or problems, nursing diagnosis):
There is mild infection in the respiratory tract, with an aggravated inflammation of the bronchi, a pain in breathing whenever the patient encounters any allergy like dust or smoke. The patient is allergic to dust, mostly due to the asthma.
Recommendation (diagnostic evaluation, follow-up care, patient education teaching including health promotion education):
The patient should;
Avoid environments with allergies, like dust and smoke
Correct use of asthma drugs as prescribes by the doctor
Avoid stress related causes to remain depression free and avoid aggravated and deep headache.
Nursing Functional Health Pattern Assessment
CLIENT: TOM TERICK
AGE: 17
Ordered and selected data Nursing diagnostics Goals Interventions
Rationale Evaluation
Subjective data; the client says he feels weak, lying in bed, while vomited thrice. Requested to go to bathroom. Showed signs of weakness while tends to lie in one position. Cold on touch. The peripheral pulsed diminish in lower extremities. Prolonged vomiting relates risk of injury related to weakness. Probability of dehydration due to altered tissue perfusion. Defined characteristics are;
Altered nobility
Weakness
Fatigue
A
Altered perfusion of peripheral tissue Short term: the client will discuss on the importance of reaching out to an ambulance on 01/17/17
Long term: the client will be proven injury free on 14/07/17 Independent:
Assessment of muscle strength, while sharing findings with client
Assessment orientation
Expression of emotion by the client
Ask client to us bell or ask for any assistance until strength is fully given
Keep a safe environment for the client Determines a cognitive ability of the client
Determines the tolerance ability of the client
Client awareness determination
Promotes safety
Promoted awakened on personal condition by the client
Promotes safety generating guidance on care giving. Short time met goals:
Client stated feeling weaker than before, and asked for help in getting up
Long time goals met:
Client has sustained no injury.
Cite this page
Health History and Examination - Paper Example. (2021, Jul 02). Retrieved from https://midtermguru.com/essays/health-history-and-examination-paper-example
If you are the original author of this essay and no longer wish to have it published on the midtermguru.com website, please click below to request its removal:
- Professionalism in Nursing - Essay Example
- Mental and Material Manifestations of Spatial Injustices in Sub-Saharan Africa - Paper Example
- Essay Sample on Conspiracy Theories: Do Vaccines Cause Autism?
- Nursing Professionals: Bridging Access to Healthcare for Underserved Communities - Essay Sample
- Tailor-Made Solutions: Healthcare Professionals Embrace Case Management for Diabetes - Essay Sample
- Pernicious Anemia: Causes, Symptoms, & Treatments - Research Paper
- Similarities in The Bear Came Over The Mountain and Away From Her - Essay Sample